Building AI-powered healthcare platforms sounds exciting, but the reality is messy. How to manage sensitive patient information and remain effective in using AI. HIPAA rules are not properly comprehended by many teams that fall into AI integration solutions without proper knowledge, resulting in leaked data, a lack of compliance, and legal liabilities.
This is normally occurring since the developers are more concerned with speed and innovations rather than security, governance, and healthcare rules. And with the incorporation of complex cloud systems and third-party tools, it becomes even more difficult to manage.
However, by focusing on HIPAA compliance software at the earliest stage, including data security, access control, AI management, and the infrastructure, it is possible to create powerful AI health platforms that can be considered innovative but safe at the same time.
According to an expert guide on HIPAA, AI integration must be done with technical, administrative, and contractual safeguards to meet HIPAA standards. In this blog, we’ve explored all you need to know about building HIPAA compliant AI health platform and more.
Key Takeaways
- The security-first architecture is the basis of developing AI-based health solutions that meet the requirements of HIPAA regulations.
- The system must be designed to comply with HIPAA-compliant AI platforms, rather than to accomplish it subsequently.
- A responsible AI practice is important. With anonymised, well-controlled healthcare data, it will be possible to minimise the privacy risks and preserve correct and solid AI results.
- A proper platform can accommodate new users, features, and integrations without violating security or regulatory standards.
Why AI-Native POCs Matter in Field Care and Health Logistics?
With the transition of healthcare provision out of hospitals and into homes and fields, AI-native Proofs of Concept are essential to affirm the safety, compliance, and practical reliability first before the full-scale development of the platform.
- The increasing complexity of decentralized healthcare delivery: Healthcare has become associated with mobile clinicians, home diagnostics, ambulance networks, and distributed labs. AI-native POCs facilitate testing data flows, latency, and coordination between fragmented systems in which downtime, misrouting, or delays have a direct negative effect on patients.
- The failure of traditional MVPs in health settings: Traditional MVPs concentrate on features and speed without paying much attention to compliance, audit trails, and edge case failures. In the healthcare field, this strategy fails fast since AI systems have to work on a consistent basis at the onset, within regulatory, clinicall and operational limits.
- POC vs. MVP: what medical teams ought to prove at first: The POCs in healthcare must confirm data safety, consent management, model precision in the sphere, and recovery of failures. MVP developemnt comes later. Regulatory safety and operational trustworthiness are more important than interfaces or features.
Why a HIPAA-Compliant POC Saves Time, Cost, and Risk?
A HIPAA-compliant app development proof of concept helps healthcare teams test AI ideas, avoid legal trouble, and reduce rework before moving to full-scale development or real patient use.
- Faster validation without rework: Building compliance into the POC ensures security and privacy are tested early. This prevents redesigning the entire system later, saving months of development time and avoiding delays during audits or approvals.
- Lower development and compliance costs: A compliant POC highlights risks and gaps before full investment. Fixing issues early is far cheaper than correcting security flaws or legal problems after launch, especially in healthcare AI products.
- Reduced legal and data-breach risk: HIPAA-ready POCs protect patient data from day one. This minimizes the chance of data leaks, fines, or trust loss, helping teams confidently move from testing to real-world deployment.

What Makes Health-Logistics POCs Fundamentally Different?
Health-logistics POCs are inherently unlike typical prototypes in that they exist in the care setting environment, where errors, delay, or data gaps may have a direct effect on patient safety and compliance.
1. Use Cases of High-Risk, High-Compliance: Health-logistics POCs assist in the controlled workflows in which the accuracy, auditing, and security are imperative so that the clinical decision-making, data management, and functions comply with rigid healthcare and privacy standards.
2. Mobile Clinicians, Home Care, Emergencies, and Handoffs of Assets: Such POCs have to operate in a reliable manner even in spread-out locations, allowing smooth coordination between field clinicians, care teams and medical assets without relying on fixed infrastructure.
3. Live Reaction with Data Loss Wasting: Logistics in health care demand real-time data and access, as any delays or lack of data may interfere with care services, compromise compliance, and undermine patient care.
Core Capabilities to Validate in a Field Care POC
To develop an AI app that would be HIPAA compliant, you have to begin by verifying the appropriate capabilities in your Field Care POC to make sure that the system would be safe, reliable, and practically useful to clinicians and patients.
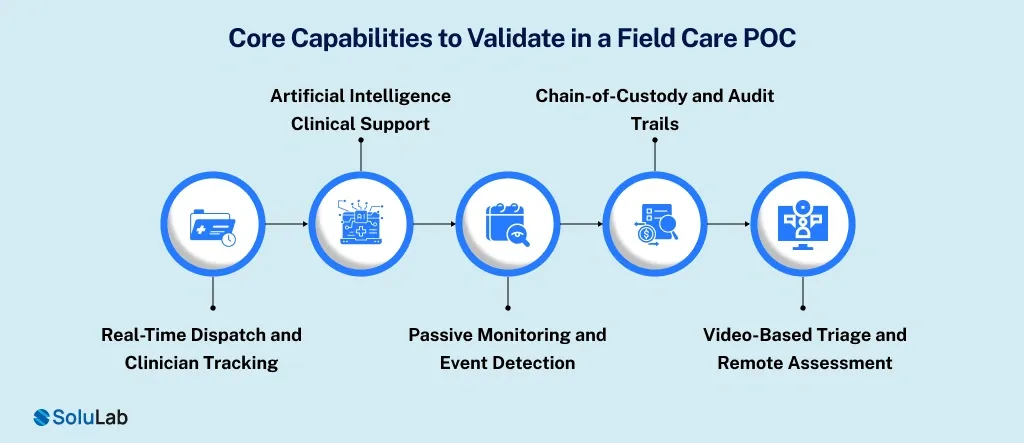
1. Real-Time Dispatch and Clinician Tracking: The site must be able to handle real-time location tracking, intelligent routes, and live status updates of clinicians. It will guarantee response time, coordination, and total visibility in case of emergency or in-home care visits.
2. Artificial Intelligence Clinical Support: AI should be used to aid clinicians in symptom assessment, clinical advice, and decision making, but not to substitute the clinician. To establish trust and accountability, models must operate safely, model with conforming data, and provide interpretable results.
3. Passive Monitoring and Event Detection: The system must also be able to monitor vitals or sensor data in the background, detecting irregularities such as falls or unexpected health changes. Alerts should have real-time activation and show the accuracy of data, patient approval, and low false positives.
4. Chain-of-Custody and Audit Trails: All data transactions, such as access, modification, or transfer, must be automatically logged. Effective audit trails guarantee HIPAA compliance, assist with legal review, and bring transparency among care teams, vendors, and regulatory stakeholders.
5. Video-Based Triage and Remote Assessment: Secure and encrypted video can be used to conduct real-time remote diagnostic and triaging. The POC must authenticate low-latency streaming, clinical-quality visuals, and smooth documentation, and guarantee patient privacy and safe data storage during sessions.
Designing the Right POC Architecture
To develop an AI health platform that is HIPAA-compliant, it is important to start with a robust POC system that can ensure both security and usability as well as scalability, and that protects patient data as the product expands.
1. API-First Mobile and Web Interfaces: Work with an API-first approach to ensure that mobile applications, web dashboards, and third-party solutions all communicate via a shared security layer. This means that there would be consistent access to data, easier updates, and greater control of authentication and permissions.
2. Protect Data During Cross-Stack Data Transfers: Encrypt data at all phases- storing, transferring, processing, and so on. Role-based access should be used to ensure sensitive dataise only visible to the authorised users. In addition, keep audit logs, which will show who accessed data and when.
3. Scaling Technology Choices Beyond the POC: Select cloud computing, data storage, and generative AI tools that are HIPAA-compliant and scale. Avoid shortcuts. The tools that perform well in a demo should also have the capacity to support greater volumes of data, an increase in the number of users, and stricter compliance in the future.
POC Engagement and Ownership Models for HealthTech Teams
A quality healthcare app development is based on HIPAA and begins with clear POC ownership. The right engagement model can assist HealthTech teams in risk reduction, data protection, and safe and fast movement.
- Fixed-Scope, Milestone-Driven POC Development: The scope, schedule, and deliverables of the POC are well defined in this model. The milestones are set every time work is done, and progress is easily monitored. It assists HealthTech teams to keep costs in check, prevent scope creep, and keep within compliance objectives.
- IP Ownership and Risk Reduction: The initial ownership of the AI model, code, and data is determined by the clear rules of IP ownership. This will minimize the legal risk, prevent future controversies, and make sure that patient data remains secure,e increasing the scale of the platform once the POC is successful.
How SoluLab Streamlines HIPAA-Compliant AI Health Platforms?
SoluLab simplifies the complex process of building HIPAA-compliant AI health platforms by combining secure architecture, smart AI practices, and healthcare-grade compliance into one clear, scalable technical approach.
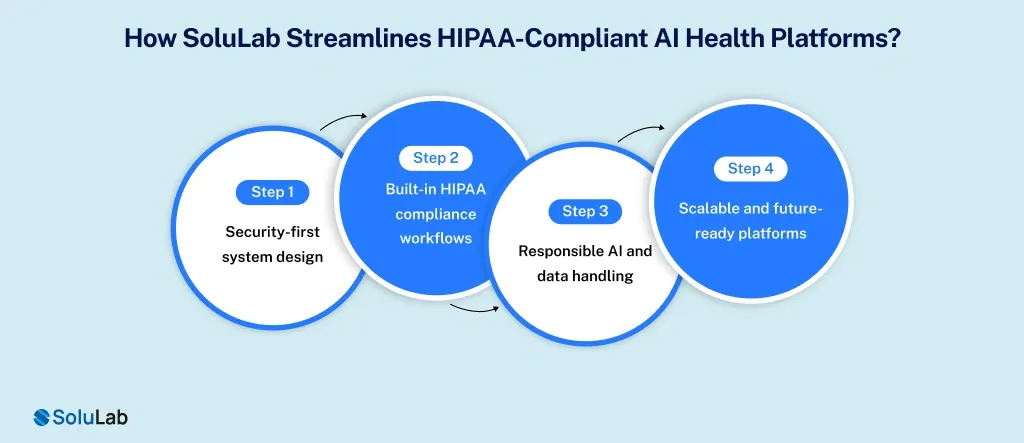
1. Security-first system design: SoluLab builds platforms with encryption, secure cloud infrastructure, access controls, and audit logs from day one. This keeps the data of patients secure when at rest, in transit, and during AI processing.
2. Built-in HIPAA compliance workflows: They map HIPAA rules directly into the system architecture. This includes role-based access, activity tracking, automatic logging, and compliance-ready documentation to support audits and regulatory reviews.
3. Responsible AI and data handling: SoluLab utilises clean, anonymised, and well-managed healthcare information as AI models. This minimizes the privacy risks and makes AI outputs accurate, ethical, and healthcare-compliant.
4. Scalable and future-ready platforms: Their AI health platforms are designed to scale safely as user numbers grow. Updates, new features, and integrations can be added without breaking security or compliance standards.

Conclusion
The development of an AI health platform that complies with HIPAA can be a daunting task, but it is actually a matter of simplicity: you need to get the basics of security, compliance, and responsible AI design right.
With privacy planned at the very first stage, secure infrastructure, and patient data in responsible hands, innovation will be a lot safer. It is only when trust is incorporated into the system that AI can be able to truly enhance healthcare. Just as we did in a project for clinical decision making.
SoluLab, a leading AI Development company, can help you HIPAA compliant AI health platform from scratch. Book a free discovery call today to discuss further!
FAQs
The HIPAA safeguards any identifiable health data, such as medical records, test outcomes, names of patients, addresses, or any other information that is connected to a patient’s health status.
Encryption is really important for information. It keeps this information safe so that only the right people can see it. When we store information or send it to other systems or computer programs, encryption makes sure that unauthorized individuals cannot get to it.
Yes, cloud hosting is permitted provided that the provider is capable of supporting HIPAA requirements and provides a secure infrastructure, as well as signing a Business Associate Agreement (BAA).
Yes, startups can build compliant platforms by following secure design principles, using compliant tools, and working with healthcare and compliance experts early.
The security tests are to be conducted regularly, particularly following the system upgrades, the introduction of a new AI feature, or modifications in the infrastructure that may influence the security of data.




